High Copay
*Terms and Conditions apply. This benefit covers HUMIRA® (adalimumab) alone or, for rheumatology patients, HUMIRA plus one of the following medications: methotrexate, leflunomide (Arava®), or hydroxychloroquine (Plaquenil®). Eligibility: Available to patients with commercial prescription insurance coverage for HUMIRA who meet eligibility criteria. Co-pay assistance program is not available to patients receiving prescription reimbursement under any federal, state, or government-funded insurance programs (for example, Medicare [including Part D], Medicare Advantage, Medigap, Medicaid, TRICARE, Department of Defense, or Veterans Affairs programs) or where prohibited by law or by the patient’s health insurance provider. If at any time a patient begins receiving prescription drug coverage under any such federal, state, or government-funded healthcare program, patient will no longer be able to use the HUMIRA Complete Savings card and patient must call HUMIRA Complete at 1-800-4HUMIRA to stop participation. Patients residing in or receiving treatment in certain states may not be eligible. Patients may not seek reimbursement for value received from the HUMIRA Complete Program from any third-party payers. Offer subject to change or discontinuance without notice. Restrictions, including monthly maximums, may apply. Patients who are members of insurance plans that claim to reduce or eliminate their patients' out of pocket co-pay, co-insurance, or deductible obligations for certain prescription drugs based upon the availability of, or patient's enrollment in, manufacturer sponsored co-pay assistance for such drugs (often termed 'maximizer' programs) will have an annual maximum program benefit of $6,000.00 per calendar year. This assistance offer is not health insurance. To learn about AbbVie’s privacy practices and your privacy choices, visit www.abbvie.com/privacy.html
High copays are perfectly acceptable for medically non-indicated or frequently overused services or for high-cost drugs, if less expensive, equally effective alternatives are available. Copays affect different populations differently. . A copay applies for any care received for a medical condition that’s treated or monitored during a preventive visit. We follow the Centers for Medicare & Medicaid Services (CMS) Medicare. Coverage and coding guidelines for all network services. You can view Coverage Summaries on UHCprovider.com.
Arava and Plaquenil are registered trademarks of their respective owners.
A smart pick if you take brand-name prescription drugs.
New: A $600 Medicare Part B premium reimbursement.

You work hard to maintain your health and live a healthy lifestyle. In 2020, count on GEHA’s High Option plan to support you on your wellness journey.
Maybe you depend on brand-name prescription medications. Maybe you’re a Medicare A&B enrollee looking for a $600 reimbursement to help with your Medicare Part B premium payments. Maybe you’ve simply reached that point inlife where you’re willing to spend a little more for a premium plan that gives you the confidence to live life to its fullest. High Option was designed with you in mind.
When you enroll in GEHA’s High Option, you’ll get:
- Comprehensive prescription coverage that works with Medicare.
- Get a $2,500 hearing-aid allowance.
More High Option highlights:
- Combines a $600 reimbursement for Medicare Part B premiums with a cost-share waiver, making High Option the plan of choice of Medicare enrollees.
- Low out-of-pocket costs when you need care.
- Similar to other plans, you get worldwide coverage that lets you travel abroad worry-free.
2020 Rates
These rates do not apply to all enrollees. If you are in a special enrollment category, please refer to the FEHB Program website or contact the agency or Tribal Employer that maintainsyour health benefits enrollment.
| Self Only | Self Plus One | Self and Family | |
|---|---|---|---|
| Non-Postal biweekly | $105.42 | $246.51 | $304.39 |
| Postal biweekly – Category 1 | $102.14 | $239.51 | $296.80 |
| Postal biweekly – Category 2 | $92.32 | $218.50 | $274.04 |
| Monthly (retirees) | $228.41 | $534.11 | $659.51 |
The combination of a $600 reimbursement for Medicare Part B premiums with a cost-share waiver, makes the High Option the plan of choice for Medicare enrollees.
In-network doctor visit copays are an affordable $20.
You can get 30-day supplies of generic drugs for just $10.
High Copay Means
Limit your out-of-pocket costs for specialty prescriptions and preferred brand-name medicines.
PreviousNextCosts for services in 2020
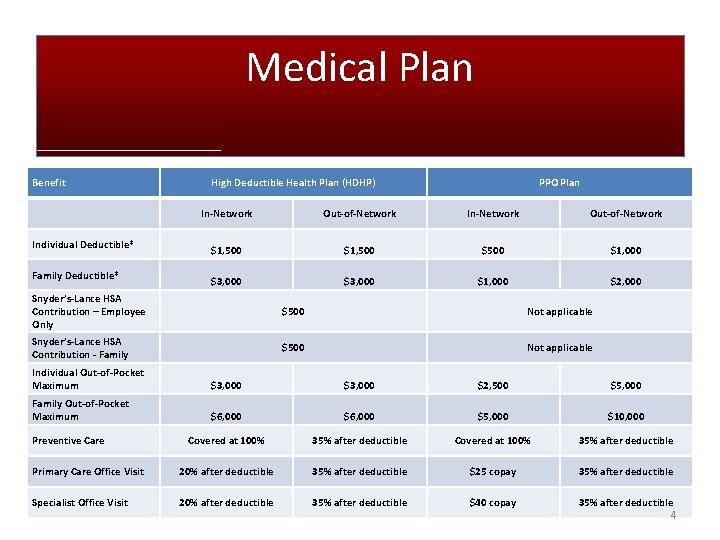
The table below summarizes your in-network cost for medical benefits with GEHA High Option. For complete information, refer to the GEHA Plan Brochure.
Copays
| Copay | What you pay in-network |
|---|---|
| Primary physician office visit | $20 |
| Specialist | $20 |
| MinuteClinic (where available) | $10 |
| Urgent care | $35 |
| Routine eye exam | $5 through EyeMed |
Other services
| Service | What you pay in-network |
|---|---|
| Preventive lab services | Nothing with Lab Card |
| Well-child visit; up to age 22 | Nothing |
| Adult routine screening | Nothing |
| Preventive dental care | Balance after GEHA pays $22/visit, twice yearly |
Maternity care
| Service | What you pay in-network |
|---|---|
| Routine provider care | Nothing |
| Inpatient care | Nothing |
| Self Only | Self Plus One | Self and Family | |
|---|---|---|---|
| Calendar-year deductible (in-network) | $350 | $700 | $700 |
| Out-of-pocket-maximum (in-network) | $5,000 | $10,000 | $10,000 |
Prescriptions
The table below summarizes your cost for prescription drugs with GEHA’s High Option. For complete benefit information, including details on specialty drugs that are injected or infused, refer to the GEHA Plan Brochure.
To find a drug cost based on your benefit plan and prescription dosage, check your drug costs.
Retail pharmacy – 30-day supply
| In-network | Out-of-network | |
|---|---|---|
| Generic | $10 copay‡ | $10 copay‡# plus difference between plan and drug cost |
| Preferred brand-name | 25%, up to $150 max‡¤ | 25%, up to $150 max‡¤# |
| Non-preferred brand-name | 40%, up to $200 max‡¤ | 40%, up to $200 max‡¤# |
Mail service pharmacy – 90-day supply
| In-network | Out of-network | |
|---|---|---|
| Generic | $20 | n/a |
| Preferred brand-name | 25%, up to $350 max¤ | n/a |
| Non-preferred brand-name | 40%, up to $500 max¤ | n/a |
‡Costs for initial prescription and first refill. You pay 50% for third and additional refills at retail for 30-day supply. For long-term prescriptions, use mail order or your local retail CVS Pharmacy store (90-day supply) for greater cost savings.

¤If you choose a brand-name medication when a generic is available, you will be charged the generic copay plus the difference in cost between the brand-name and the generic.
#Your claim will be calculated on the coinsurance or the appropriate copayments. Reimbursement will be based on GEHA’s costs had you used a participating pharmacy. You must submit original drug receipts.
HEARING-AID DISCOUNTS
VISION COVERAGE
MEDICAL ALERT SYSTEM
^GEHA supplemental benefits are neither offered nor guaranteed under contract with the FEHB, but are made available to all enrollees and family members who become members of a GEHA medical plan. For information on year-round savings for GEHAdental members, visit Savings for GEHA dental members.
High Copayment
Help With Insurance Copays
View Results